Ingrown Toenail Management
 An ingrown toenail occurs when the edge of a toenail grows into the surrounding skin, causing pain, swelling, and sometimes infection. This condition is often seen in the big toe and can result from improper nail trimming, wearing tight footwear, or injury to the toe. When the nail pierces the skin, it creates an entry point for bacteria, leading to redness, pain, and pus formation. Managing an ingrown toenail involves soaking the affected foot in warm water to reduce swelling, gently lifting the nail edge, and applying antibiotic ointment. It is important to avoid cutting the nail too short or rounding the corners, as this can worsen the condition. Complications from untreated ingrown toenails can include severe infections, abscess formation, and in extreme cases, bone infections. To prevent ingrown toenails, trim nails straight across, wear properly fitting shoes, and maintain good foot hygiene. If the condition persists or worsens, it is suggested that you
An ingrown toenail occurs when the edge of a toenail grows into the surrounding skin, causing pain, swelling, and sometimes infection. This condition is often seen in the big toe and can result from improper nail trimming, wearing tight footwear, or injury to the toe. When the nail pierces the skin, it creates an entry point for bacteria, leading to redness, pain, and pus formation. Managing an ingrown toenail involves soaking the affected foot in warm water to reduce swelling, gently lifting the nail edge, and applying antibiotic ointment. It is important to avoid cutting the nail too short or rounding the corners, as this can worsen the condition. Complications from untreated ingrown toenails can include severe infections, abscess formation, and in extreme cases, bone infections. To prevent ingrown toenails, trim nails straight across, wear properly fitting shoes, and maintain good foot hygiene. If the condition persists or worsens, it is suggested that you
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Lesly Honore, MD, DPM of New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Hempstead, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
Causes of Toe Swelling

Toe swelling can result from a variety of causes, ranging from minor issues to more serious health conditions. One common cause is injury, such as stubbing your toe or dropping something heavy on it, which can lead to bruising and swelling. Infections, including fungal infections like athlete's foot or bacterial infections, can also cause swelling and redness. Arthritis, particularly gout, is another culprit, often leading to painful, swollen toes due to the buildup of uric acid crystals. Poor circulation, which can be associated with conditions like diabetes or peripheral artery disease, may cause fluid buildup in the toes, resulting in swelling. Additionally, wearing ill-fitting shoes that pinch or put pressure on the toes can lead to swelling and discomfort. If you have swollen toes, it is suggested that you consult a podiatrist who can determine what the cause is, and offer appropriate treatment solutions.
Toe pain can disrupt your daily activities. If you have any concerns, contact Lesly Honore, MD, DPM of New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Hempstead, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
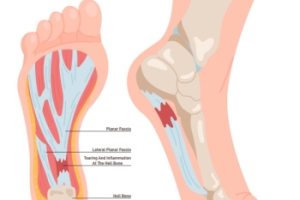
The Pain of Plantar Fasciitis
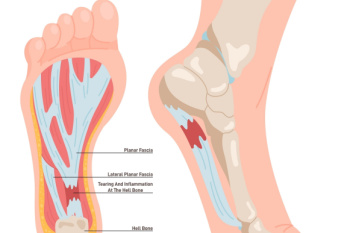 Plantar fasciitis causes heel pain, resulting from inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of the foot and connects the heel bone to the toes. It typically occurs due to repetitive strain or overuse, often seen in runners, individuals with high arches or flat feet, and those who stand for prolonged periods. The pain from plantar fasciitis is usually sharp and most intense with the first steps in the morning or after periods of inactivity. It may decrease with movement but can return after long periods of standing or walking. Relief can consist of rest, stretching exercises, and taking anti-inflammatory medication. Wearing supportive shoes and using orthotic inserts can also help. Preventative measures involve maintaining a healthy weight, performing regular foot stretches, and avoiding excessive strain on the feet. If left untreated, plantar fasciitis can lead to chronic heel pain and other complications. If you have heel pain, it is suggested that you visit a podiatrist for a proper diagnosis and an effective treatment plan.
Plantar fasciitis causes heel pain, resulting from inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of the foot and connects the heel bone to the toes. It typically occurs due to repetitive strain or overuse, often seen in runners, individuals with high arches or flat feet, and those who stand for prolonged periods. The pain from plantar fasciitis is usually sharp and most intense with the first steps in the morning or after periods of inactivity. It may decrease with movement but can return after long periods of standing or walking. Relief can consist of rest, stretching exercises, and taking anti-inflammatory medication. Wearing supportive shoes and using orthotic inserts can also help. Preventative measures involve maintaining a healthy weight, performing regular foot stretches, and avoiding excessive strain on the feet. If left untreated, plantar fasciitis can lead to chronic heel pain and other complications. If you have heel pain, it is suggested that you visit a podiatrist for a proper diagnosis and an effective treatment plan.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Lesly Honore, MD, DPM from New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Hempstead, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
A Surgical Procedure for Plantar Fasciitis

Endoscopic plantar fasciotomy, or EPF, is a surgical procedure used to treat plantar fasciitis. This painful foot condition is caused by inflammation of the thick band of tissue that runs along the bottom of the foot, known as the plantar fascia. During an EPF procedure, a small incision is made in the foot, and a thin, tube-like instrument called an endoscope is inserted to visualize the plantar fascia. Using specialized instruments, the podiatrist then cuts or releases the tight or damaged portion of the plantar fascia, relieving tension and reducing pain. Unlike traditional open surgery, EPF is minimally invasive and typically results in less postoperative pain, faster recovery times, and smaller scars. This procedure is often recommended for patients who have not responded to conservative treatments, such as rest, orthotic devices, or steroid injections. If you have plantar fasciitis, it is suggested that you are under the care of a podiatrist who can determine if this type of surgery is right for you.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Lesly Honore, MD, DPM of New York. Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Hempstead, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Cuboid Syndrome in Athletes
 Cuboid syndrome is a condition where the cuboid bone, located on the outer side of the midfoot, becomes partially dislocated or misaligned. This often occurs due to injury or repetitive strain. Athletes are more likely to get cuboid syndrome than other groups because their activities, such as running or jumping, put significant stress on the foot's complex structures. This is especially true for those in sports requiring sudden changes of direction or explosive movements. Symptoms of cuboid syndrome may include intense lateral foot pain, redness, and swelling. A podiatrist, or foot doctor, can treat cuboid syndrome through manual manipulation to realign the bone, along with rest, compression, and elevation to reduce inflammation. Additionally, the use of taping techniques and custom orthotics may help stabilize the cuboid bone and prevent recurrence, allowing athletes to return to their activities with reduced risk of further injury. If you suspect cuboid syndrome, it is suggested you make an appointment with a podiatrist as soon as possible.
Cuboid syndrome is a condition where the cuboid bone, located on the outer side of the midfoot, becomes partially dislocated or misaligned. This often occurs due to injury or repetitive strain. Athletes are more likely to get cuboid syndrome than other groups because their activities, such as running or jumping, put significant stress on the foot's complex structures. This is especially true for those in sports requiring sudden changes of direction or explosive movements. Symptoms of cuboid syndrome may include intense lateral foot pain, redness, and swelling. A podiatrist, or foot doctor, can treat cuboid syndrome through manual manipulation to realign the bone, along with rest, compression, and elevation to reduce inflammation. Additionally, the use of taping techniques and custom orthotics may help stabilize the cuboid bone and prevent recurrence, allowing athletes to return to their activities with reduced risk of further injury. If you suspect cuboid syndrome, it is suggested you make an appointment with a podiatrist as soon as possible.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Lesly Honore, MD, DPM from New York. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our office located in Hempstead, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cuboid Syndrome
Cuboid syndrome mostly affects athletes, although it can affect non-athletes too. It is also known as cuboid subluxation or cuboid fault syndrome. This condition occurs when joints and ligaments near the cuboid bone of the foot are damaged, or when the cuboid bone itself is dislodged from its natural position. It is usually marked by pain on the outer side of the foot, which may be persistent or may come and go. Cuboid syndrome can be difficult to diagnose unless it becomes severe and more noticeable. Your doctor will likely ask questions about when the pain began and how long it has been present, and will put pressure on the cuboid bone to determine if that area is the origin of the pain.
Causes of Cuboid Syndrome
- Any repetitive stresses placed on the foot due to athletic activities are a common cause of cuboid syndrome.
- Although it develops over time, it is possible that this syndrome can occur all of sudden due to a single event or injury.
- Over-pronation can exacerbate the condition if not corrected.
Disagreements Amongst Podiatrists Regarding Cuboid Syndrome
- Some refer to it as the dislocation of the calcaneal-cuboid joint only.
- Other podiatrists see it as an injury of the ligaments located nearby, which also involves the cuboid bone.
It is very important that when you experience any kind of pain on the side of your foot, you should seek medical care right away. If a subluxed cuboid is caught early, your feet may respond well to the treatment, and you can get back into sports or other activities again as soon as the pain subsides.
The Versatility of Custom Orthotics

Custom orthotics, often associated with runners or athletes, offer benefits beyond the realm of sports. These specialized shoe inserts are designed to address imbalances in foot structure, which can significantly impact posture and overall body alignment. Even a minor imbalance can lead to problems throughout the body. Orthotics may be beneficial if you notice uneven wear on the soles of your shoes or have frequent ankle sprains. Chronic pain in the heels, misaligned toes, or abnormal foot positioning during walking are other reasons that orthotics may be needed. By providing support and stability, orthotics help distribute weight more evenly across the foot, reducing strain on muscles and joints. They can correct biomechanical issues, improve gait efficiency, and alleviate discomfort associated with various conditions. Whether you are an athlete or someone seeking relief from everyday discomfort, custom orthotics offer a simple yet effective solution to enhance foot function and promote overall well-being. If you are interested in learning more about how custom-made orthotics can help you, it is suggested that you consult a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact Lesly Honore, MD, DPM from New York. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Hempstead, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.